
O Routine physicals and most screening tests O Services paid for by a government entity other than Medicare (this exclusion does not include services paid for by Medicaid on behalf of dual-eligibles) O Services for which there is no legal obligation to pay
E1399gylt statutorily excluded manual#
Medicare Claims Processing Manual (MCPM) Chapter 30 Financial Liability Protections states the following:
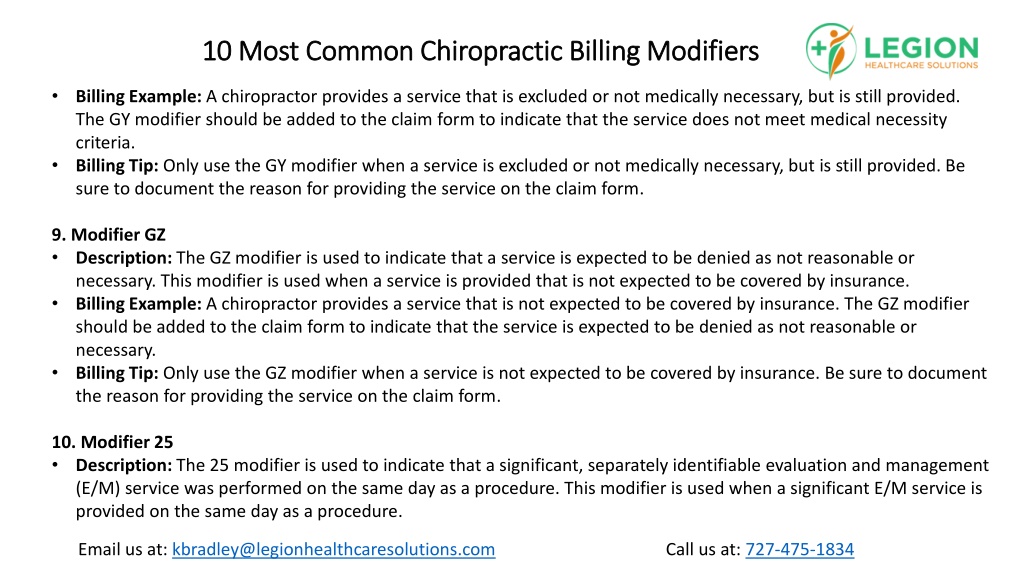
The definition is for GY is it is to be used for items or services that are statutorily excluded items or that do not meet the definition of any Medicare benefit. SSA §1862(a)(1) of the Act (not reasonable and necessary) requires that an ABN be used for all of the National Coverage Decisions without coverage… If you have been a little liberal with your sprinkling of the GY Modifier consider the following:
The research I conducted made me realize that using the GY modifier instead of issuing an ABN is very limited. After much debate in the office I work in, I decided to write an ABN/Modifier policy, based on regulations, that we all could live with.


 0 kommentar(er)
0 kommentar(er)
